“Oh, you have type 1 diabetes! So you have to inject insulin every day?”
If only living with T1D was as simple as just injecting some insulin every day, like taking a pill or watering the plants. Instead, injecting insulin is more like administering your own anaesthetic – too little and you suffer, too much and your dead. Insulin is potent stuff and the margins are narrow.
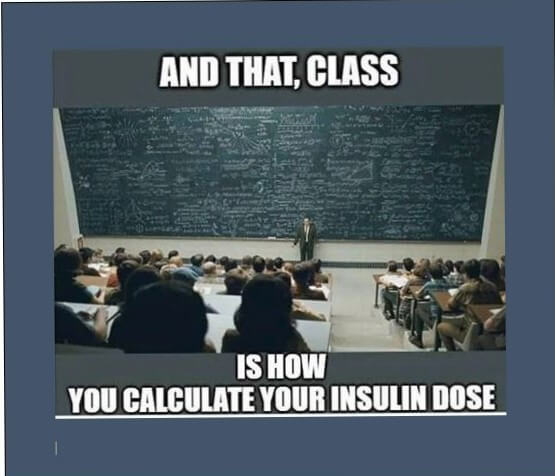
The most difficult bit though is calculating your insulin dose. Why? Because so many variables affect blood sugars, and they all interact in endlessly subtle and complex ways.
“How much insulin should I inject for this later-than-usual dinner with a glass of wine after a hot day outside and a long run yesterday?”

I hope this list does two things: reminds people with T1D that it’s OK not to have perfect blood sugars – it’s not your fault, because the multitude of variables just makes blood sugars impossible to predict and control with perfect precision. On the flip side, understanding this list gives you the power to control your blood sugars better – every variable is an opportunity to control the controllable and improve your blood sugars.
Remember that even if you don’t have diabetes, many of these factors still affect your blood sugars. As well as being beneficial for your health, having fewer blood glucose excursions reduces hunger, mood swings and fatigue.
Food
- Quantity of carbohydrates. The most obvious one. Eating three slices of bread will raise blood sugar levels more than eating one.
- Glycemic index of carbohydrates– read this article to find out more. Factors that have an effect include the type of carbohydrate, fat content, protein content, cooking method, processing, surface area, acidity and fibre content!
- Meal timing – due to the diurnal endocrine variation (daily hormone cycle), the time meals are eaten has an effect on the glycemic response. [i]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1633483/.
- Dehydration – causes increased blood glucose levels due to simple hemoconcentration of blood glucose, decreased renal glucose clearance, and possibly from enhanced counterregulatory hormone secretion in the dehydrated state [ii]https://www.sciencedirect.com/science/article/pii/S0026049501321571
- Alcohol – Alcohol is well-known to decrease blood sugar levels but the scientific evidence is lacking – an in-depth review coming soon! [iii]https://onlinelibrary.wiley.com/doi/full/10.1002/dmrr.2965?casa_token=FLpy7TDM-BQAAAAA%3AeembpOj-3ogXkBPDFl9inwRgSNS5fMIZuwfO3CqixaYBsvj0O2Yu0TA1Z-HM0XktEK1Dmy7m0MnBPmRM
- Caffeine – mixed-effects [iv]https://www.sciencedirect.com/science/article/pii/S1871402117300966?casa_token=K29-nqua4kMAAAAA:bH3OxutLJOO8xYxbj4saFJijnIp74eG2eUuzNmhFBW9I0pZQl3ABRBOiapM_MhRiUsCtGnI81w.
Insulin
- Dosage – how much insulin you inject.
- Type – which type of insulin analogue you inject and what analogues you use.
- Timing – in relation to all the other factors, particularly food and physical activity. Insulin action has a peak (different for each type of insulin) [v]https://www.liebertpub.com/doi/abs/10.1089/dia.2009.0112.
- Site of injection – absorption rates differ across the body.[vi]https://www.hindawi.com/journals/jdr/2018/1205121/
- Subcutaneous blood flow – temperature, exercise, obesity, body position, blood pressure, use of vasodilating/vasoconstricting drugs, and smoking all influence rate of insulin absorption. [vii]https://www.hindawi.com/journals/jdr/2018/1205121/
Physical activity
Exercise causes enhanced muscle insulin sensitivity via increased activation of non-insulin sensitive glucose transporters. During exercise, the dramatic increase in non-insulin-mediated glucose disposal considerably reduces the need for circulating insulin levels.
- Intensity – light vs aerobic vs anaerobic. Light exercise such as walking causes a disproportionate fall in blood glucose as it doesn’t stimulate the counter hormonal response. Anaerobic exercise like resistance exercise usually causes an increase in blood glucose due to an adrenaline response that releases stored glucose [viii]https://diabetesjournals.org/care/article/36/3/537/38023/Resistance-Versus-Aerobic-ExerciseAcute-effects-on [ix] … Continue reading
- Duration – the longer the exercise duration the greater the fall in blood glucose
- Type of sport – every sport has slightly different physiological demands and thus different effects on blood sugars.
- Time of day – interaction with diurnal endocrine variation
- Timing with food – physical activity redirects blood flow away from the digestive system, slowing the absorption of carbohydrates. [x]https://journals.humankinetics.com/view/journals/ijsnem/16/5/article-p485.xml, [xi]https://jissn.biomedcentral.com/articles/10.1186/1550-2783-8-12#:~:text=Blood%20flow%20to%20central%20tissues,in%20GI%20complaints%20%5B30%5D.
- Insulin resistance from extreme exercise? – during my adventure my insulin needs more than tripled – read about this here. I can’t find any studies citing this, but I think the physical stress on my body (inflammation) could’ve caused insulin resistance from inflammation.
- Fitness level – rate of metabolism goes down as you become fitter, rate of glucose metabolism increases and glycogen storage capabilities increase [xii]https://onlinelibrary.wiley.com/doi/full/10.1111/dme.13070?casa_token=kWRxoS1svosAAAAA%3AxpzFTDldLyHcpLDqJqDtDmG1agmIonarOMZJbeTpZ3-DeQGKkp6v0tD4ygSlU9vq2uzXJdQiDS-tHYAp
- Past physical activity – exercise continues to affect insulin sensitivity for several days
Hormonal
- Puberty – hormonal changes cause insulin resistance [xiii]https://europepmc.org/article/med/11787432
- Menstrual cycle – changes in oestrogen and progesterone change resistance to insulin in unpredictable ways [xiv]https://journals.sagepub.com/doi/full/10.1177/19322968221080199
- Pregnancy [xv] … Continue reading
- Dawn phenomenon – around half of people with T1D experience insulin resistance around dawn time, caused by the release of cortisol, glucagon, epinephrine and other hormones as part of the diurnal endocrine cycle [xvi]https://link.springer.com/article/10.1007/BF00404020
- Somogyi effect – a disputed theory of post-hypoglycaemic hyperglycemia rebound caused by the hormone response to hypos [xvii]https://www.ncbi.nlm.nih.gov/books/NBK551525/
- Illness – a cocktail of hormones like adrenaline, growth hormone and cortisol released whilst ill cause insulin resistance [xviii] … Continue reading
- Psychological stress –
other factors
- Recent hypoglycemia – makes recurrent hypo more common as bodies mechanism to release glucose is blunted [xix]https://onlinelibrary.wiley.com/doi/full/10.1002/dmrr.450?casa_token=XwI-rVwIbo0AAAAA%3AAHL8iqZ1mf6g2Rx0AExmupcMvUol1b1WBeuL2ka3oB9MWE3OO_QlIuigfiLeJL4igF2UXgdw4YVR9-YL
- Fatigue – lack of sleep makes you more insulin resistant [xx]https://www.tandfonline.com/doi/abs/10.1080/07420528.2019.1615501
- Altitude – [xxi]https://diabetesjournals.org/care/article/34/3/591/38735/Increased-Insulin-Requirements-During-Exercise-at
- Smoking and recreational drug use – nicotine increases blood sugar levels [xxii]https://www.sciencedirect.com/science/article/pii/S0163725820302230#:~:text=on%20energy%20expenditure.-,4.%20Nicotine%27s%20effects%20on%20glucose%20homeostasis,-IR%20is%20a, drugs have different effects
- Medications – steroids, birth control and other medications affect blood sugars in different ways
- Microbiome [xxiii]https://onlinelibrary.wiley.com/doi/full/10.1111/dme.13070?casa_token=kWRxoS1svosAAAAA%3AxpzFTDldLyHcpLDqJqDtDmG1agmIonarOMZJbeTpZ3-DeQGKkp6v0tD4ygSlU9vq2uzXJdQiDS-tHYAp
- Honeymoon period – the amount of endogenous insulin the body is left producing after diagnosis
- Weather/climate – heat dilates blood vessels increasing absorption of insulin [xxiv]https://www.diabetesqld.org.au/news/hot-weather-can-affect-your-diabetes/
- Prior high blood glucose levels – cause glucotoxicity and insulin resistance [xxv]https://www.researchgate.net/publication/26784490_Problems_associated_with_glucose_toxicity_Role_of_hyperglycemia-induced_oxidative_stress
References
Leave a Reply